Selecting your baby's gender through IVF involves the use of pre-implantation genetic testing (PGT), a procedure that evaluates embryos for sex chromosomes with almost perfect accuracy. This occurs at the blastocyst stage, allowing parents to choose embryos of a specific gender before implantation. While this technology offers significant control, it also raises ethical questions and considerations about societal impacts, clinic policies, and what happens to unused embryos. What follows is a deeper exploration of these complexities.
Key Takeaways
- Pre-implantation genetic testing (PGT) is essential for determining embryo sex during the IVF process.
- PGT examines embryos at the blastocyst stage to assess chromosomal information for accurate gender selection.
- IVF with PGT offers nearly 100% accuracy in selecting the desired gender.
- Many clinics require medical justification for gender selection, emphasizing ethical considerations.
- Discuss PGT costs and options for unused embryos with your IVF clinic for informed decision-making.
Understanding the Difference Between Sex and Gender
In the domain of human biology and social constructs, distinguishing between 'sex' and 'gender' is vital for clarity in discussions about reproductive technologies like IVF. Sex refers to the biological and physiological attributes, including reproductive organs and chromosomes (XX for females, XY for males), that define individuals. Through IVF and pre-implantation genetic testing, sex selection is achievable by identifying these chromosomal markers. However, gender encompasses the roles, behaviors, and identities society attributes to individuals, which evolve over time. Gender identity is a personal development, distinct from biological sex. Misunderstanding this distinction can lead to confusion in parental expectations during reproductive choices. Recognizing these differences is essential for informed discussions, as it emphasizes that while sex can be chosen, gender identity remains a unique, evolving journey. Sperm sorting techniques like the Swim-Up method can be part of the preconception process to influence the sex of future children.
Overview of Gender Selection Through IVF
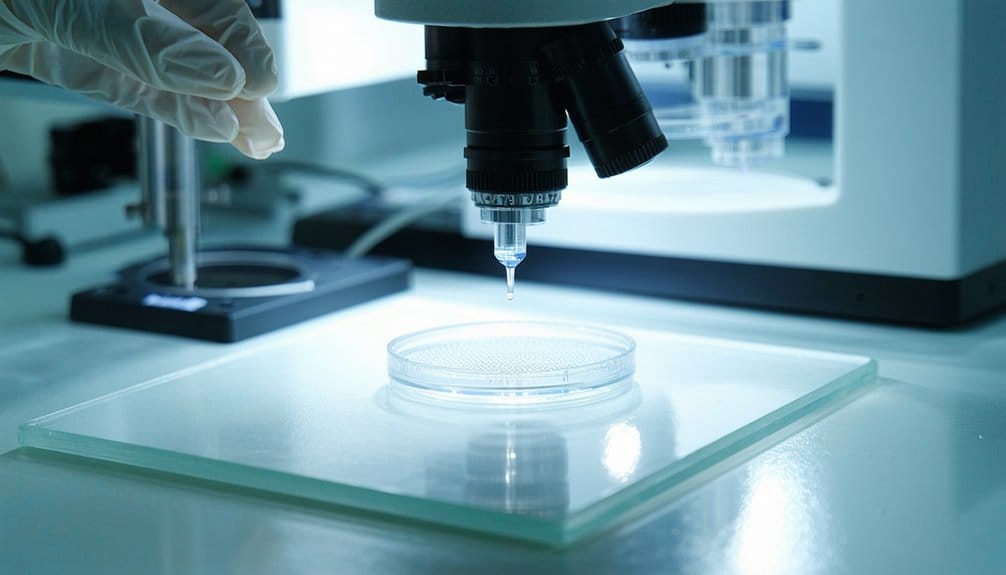
While advancements in reproductive technology have opened new possibilities for prospective parents, gender selection through IVF remains a topic of both interest and debate. Utilizing pre-implantation genetic testing (PGT), this process involves examining embryos for sex chromosomes to enable the choice of a desired gender before implantation. When embryos reach five days old, cells are removed to determine genetic information, including whether the embryo is XX or XY. This method is nearly 100% accurate, enhancing the likelihood of selecting the preferred sex. Nonetheless, ethical concerns persist, such as:
- Sex ratio imbalances that may arise globally.
- Reinforcement of gender biases within societies.
- Additional costs involved above standard IVF treatments.
Gender selection is often sought for personal preferences or family balancing, necessitating careful ethical consideration. Genetic evaluation, like PGS-PGT, can also help ensure the embryo's overall health by identifying potential genetic disorders before implantation.
Reasons for Choosing Your Baby's Gender
Parents considering gender selection through IVF often weigh health considerations and family balancing preferences. For some, the primary concern is mitigating the risk of sex-linked genetic disorders, which could considerably impact the health trajectory of their offspring. Others may seek to achieve a more balanced family dynamic, hoping to enhance familial relationships by having children of both genders.
Health Considerations in Gender
Many prospective parents consider the option of selecting their baby's gender through IVF primarily due to health-related concerns. Gender selection is often pursued to address sex-linked genetic disorders, such as hemophilia and Duchenne muscular dystrophy, which disproportionately affect one gender. Through the IVF process, preimplantation genetic testing (PGT) is utilized to screen embryos, ensuring the selection of a healthy embryo free from specific genetic disorders. This approach is particularly important for parents who have lost children to such conditions, or those with a familial history of genetic abnormalities.
- Approximately 30% of parents cite health concerns as the main reason for gender selection.
- PGT enhances the chance of selecting an embryo without sex-linked genetic issues.
- Sex-linked disorders greatly influence family planning decisions.
Family Balancing Preferences
Although some may view gender selection as a controversial practice, it is a considerable consideration for many couples seeking family balancing through IVF. Parents often desire a specific family dynamic, prompting them to choose the sex of the baby to achieve this balance. Emotional factors, such as the desire to provide siblings of the same gender or to fill the void left by a lost child, considerably influence these preferences. Cultural pressures can also play a role, as societal norms may favor one gender, affecting decisions. Additionally, gender selection via IVF can prevent sex-linked genetic disorders. Healthcare providers play a critical role in guiding couples through these decisions, ensuring that the desired sex aligns with the family's overall reproductive and emotional goals.
How Preimplantation Genetic Testing Works
Preimplantation Genetic Testing (PGT) is an essential step in the IVF process that involves the thorough analysis of embryos to assess chromosomal integrity and identify potential genetic disorders. By examining the chromosomal composition of embryos, PGT-A guarantees that they have the correct number of chromosomes, which is vital for determining both their viability and gender. This procedure not only aids in selecting a desired gender with almost complete accuracy but also helps in detecting genetic abnormalities, providing parents with an extensive understanding of their future child's genetic health.
Embryo Chromosomal Analysis
Embryo chromosomal analysis, through the use of Preimplantation Genetic Testing (PGT), plays a critical role in the in vitro fertilization (IVF) process by evaluating the chromosomal integrity of embryos. PGT identifies chromosomal abnormalities and determines sex chromosomes X and Y, facilitating gender selection before embryo transfer. This advanced reproductive technology, including pre-implantation genetic diagnosis (PGD), guarantees nearly 100% accuracy in gender selection, assuming proper analysis of viable embryos.
- PGT Process: Involves removing cells from embryos at the blastocyst stage for genetic analysis.
- PGT-A vs. PGT-M: PGT-A focuses on chromosomal health; PGT-M targets specific genetic disorders, aiding in sex selection.
- Cost Consideration: PGT is optional, adding to IVF expenses beyond standard treatment packages.
Empathetic guidance from professionals is essential throughout this process.
Genetic Disorder Identification
Genetic disorder identification in the context of in vitro fertilization is a cornerstone of preimplantation genetic testing (PGT), providing essential insights into the chromosomal health of embryos before implantation. This advanced screening process enhances the prospects of a healthy pregnancy by evaluating embryos for chromosomal abnormalities. PGT involves biopsying cells from embryos at the blastocyst stage, approximately five days post-fertilization, to assess genetic integrity. It includes PGT-A for aneuploidy, PGT-M for monogenic disorders, and PGT-SR for structural rearrangements. During this process, the sex chromosomes are also examined, allowing for gender selection with nearly 100% accuracy. Identifying XX or XY configurations enables prospective parents using IVF to make informed decisions while concurrently screening for potential genetic disorders.
Ethical Considerations in Gender Selection
The ethical landscape surrounding gender selection through IVF is a complex tapestry woven with considerations of societal impact and individual autonomy. Non-medical sex selection raises significant ethical considerations, particularly regarding gender stereotypes and societal imbalances. In cultures where one gender is preferred, this practice may exacerbate existing inequalities. Critics highlight concerns about the potential misuse of medical resources and discrimination against embryos of less preferred genders. Ethical debates stress the importance of prioritizing child well-being over gender preferences, often shaped by personal or societal pressures.
Key ethical considerations include:
- Reproductive autonomy vs. societal norms: Balancing individual choices with societal impacts.
- Informed consent: Ensuring parents understand the ethical ramifications.
- Potential reinforcement of gender stereotypes: The risk of perpetuating biases and societal imbalances.
Success Rates and Accuracy of Gender Selection
Gender selection through IVF, when paired with preimplantation genetic testing (PGT), offers an impressive near-perfect accuracy in determining the sex of embryos. This precision is achieved by analyzing chromosomal configurations to identify XX or XY embryos before implantation. Success rates of gender selection in IVF are influenced by factors such as maternal age, egg supply, and particularly sperm quality, which all affect embryo health. While the accuracy of gender selection is high, it ultimately hinges on the viability of the embryos generated during the IVF cycle. It is essential to emphasize that IVF should primarily be pursued for health reasons, such as preventing genetic disorders, rather than solely for gender preference, ensuring ethical considerations align with clinical outcomes. Technological advancements in IVF treatment have significantly improved success rates, allowing for better selection and development of healthy embryos.
Options for Unused Embryos
While the accuracy of gender selection in IVF is remarkably high, this process often results in the creation of more embryos than are needed for immediate implantation. These unused embryos present several options for parents, each with its own considerations:
- Donation: Unused embryos can be donated to other couples experiencing infertility, offering them a chance to conceive.
- Cryopreservation: Viable embryos can be frozen for future use, allowing families to expand later.
- Research: Donating embryos to medical research aids in advancing fertility science.
Ethical implications must be carefully weighed, as decisions impact both family dynamics and societal norms. Embryo donation is a process where healthy embryos are transferred to individuals in need, offering hope to those facing infertility challenges. Clear communication with fertility clinics is essential to guarantee that decisions regarding unused embryos align with personal values and circumstances, guaranteeing informed and thoughtful choices.
Discussing Gender Selection With Your IVF Clinic
Initiating the conversation begins with inquiring about pre-implantation genetic testing (PGT), a key method for identifying embryo sex with high accuracy. It's vital to understand the ethical considerations, as many IVF clinics require a medical justification for gender selection, prioritizing the birth of healthy babies. At IVOX Hospital & IVF Center, renowned for its high success rates, prospective parents can discuss personal reasons with fertility specialists to ensure advice aligns with family planning objectives. Additionally, clarity on the costs of PGT, an optional yet significant addition to the IVF process, is essential for informed decision-making. Prospective parents should also familiarize themselves with the clinic's policies on unused embryos, as these can influence future planning and ethical considerations.
Conclusion
In the domain of reproductive choices, selecting a baby's gender through IVF echoes the myth of Pandora's box, where hope and consequences coexist. Employing clinical precision and technical expertise, PGT offers near certainty in gender determination. Yet, as with any advancement, ethical reflections loom large. Steering through this terrain requires empathetic guidance, balancing personal desires with broader societal implications. Ultimately, thoughtful dialogue with IVF professionals guarantees informed decisions, respecting both scientific possibilities and the tapestry of human values.